BODY COMPOSITION, VISCERAL FAT, AND METABOLIC SYNDROME
Dr. Gabriele Bedini
Body composition, visceral fat and metabolic syndrome are the topics that we will develop in the following article. That is why we will address the topic of visceral adipose tissue, focusing the discussion on its role in the predisposition to inflammatory, cardiovascular, metabolic and eventually even oncological diseases. However, to understand it, an introduction to the mass and composition of bodies will be necessary.
Let us begin, therefore, by talking about body composition.
When we measure a person’s weight, we get a nonspecific numerical figure; in fact, that number that appears on the scale may have a different valence on different people. The first insight that will be of duty to give a more precise value to that weight, is the evaluation of the Body Mass Index (BMI) more frequently referred to in English as Body Mass Index (BMI).
Through this tool, a person’s weight is related to his or her height, resulting in a numerical value that, when applied to a scale of defined reference values, gives us a primary indication of that person’s nutritional condition.
With BMI assessment, a person’s body mass can be staged as respectively in ascending order: underweight, normal weight, overweight, obese, and classify the latter condition into the various levels of obesity (first-, second-, and third-degree also called morbid obesity, since the latter strongly predisposes to the onset of serious diseases related to body weight). Small aside: in working practice, it is surprising that several times people discover their condition of obesity, only after taking this measurement and are surprised by it, having always thought of themselves as “somewhat overweight” people.
However, BMI itself, although it is a good preliminary tool to investigate a person’s body mass, cannot be sufficient in itself to determine the real nutritional and metabolic status. For example, let us imagine 100 people who are different from each other but all have the same weight and height, the BMI will be the same for all these people, but it is not certain that all these people are “made” the same internally. In fact, it will be highly unlikely that they are.
Here, in fact, for a more precise assessment, the examination of body composition takes on a much more important role in order to be able to assess the true nutritional status of a person, and is indispensable in the practice of an examination for the proper evaluation of this parameter.
However, let us see, in essence, what body composition is.
We can first say that a person’s body is divided into two major districts representative of additional body compartments that we will see in detail later. These two main departments are: fat mass and lean mass, which we will more technically call Fat Mass (FM) and Fat Free Mass (FFM).
The Fat Mass (FM) district includes any body compartment in which there is adipose tissue, hence adipocytes (cells that contain fat). Adipose tissue can be found in different locations within a human body, we know in fact: subcutaneous adipose tissue (superficial and deep), intramuscular adipose tissue, and last but not least, VISCERAL adipose tissue of which we will discuss in detail later in this article delving into the most relevant aspects.
The counterpart of fat mass is called lean mass and is represented by “everything that is not fat” within a human body, technically in fact it is referred to as fat-free mass (FFM). In detail, this body compartment is made up of various districts: first of all and also the most quantitatively represented is precisely water (which can be intracellular or extracellular,
The measurement of body composition can be done by performing some instrumental techniques (bioimpedance and plicometry or other adipometric methods ) that we will not stay to describe in detail in this article.
hydration and water retention respectively), we then have the bones that are responsible for a person’s build, then we have the muscular district that covers an interesting function since it is metabolically more active (it plays a decisive role in making a person in good constitution and, vice versa, the lack of muscle mass known as sarcopenia, is correlated with the emaciation of a person), finally we have the soft tissues also part of the lean mass.
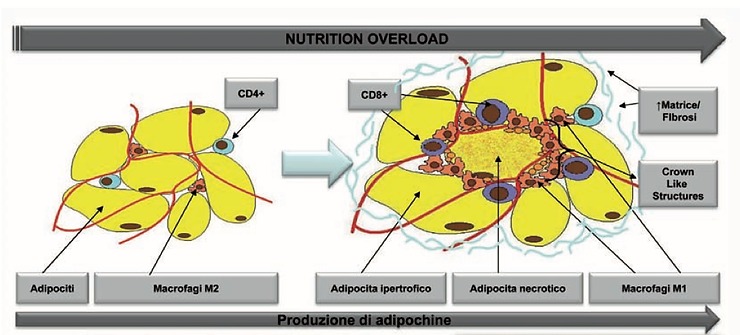
That having been done, we will now focus our attention on visceral fat, since it is the one that if expressed in a quantitatively significant amount, will play a first-order role in predisposing a person to the onset of numerous inflammatory, cardiovascular and dysmetabolic diseases. We start from the assumption that adipocytes (as already mentioned are the cells that contain fat) increase numerically only in the very early stages of development (already from before birth until the first months of life) secondary to certain types of stimuli of mostly dietary and environmental character, after which the numerical growth stops and the number of adipocytes remains almost stable throughout the rest of a person’s existence, predisposing more to the development of overweight and obesity in adulthood that subject who had developed more of them.
For this reason, if a person goes into weight gain due to fat accumulation, these fats will localize in adipocytes present in both subcutaneous and visceral locations, going on to over-saturate said adipocytes, which consequently may also reach a size considerably larger than their natural size (adipocytes, being unable to grow further in number, are naturally predisposed to increase their volume the more they are saturated by accumulated fat). This increase in adipose tissue volume, along with other factors, is one of the factors responsible for the decidedly negative effects on physical health.
In fact, the increased volume of adipose tissue results in a kind of resistance, both to the functioning of insulin and to blood flow. The blood vessels, in fact, will make it difficult to properly supply the tissue, and from this poor blood supply, a condition of hypoxia will ensue, that is, the lack of oxygen within the cells, hence the tissue. From this condition of hypoxia and distress (tissue stress) results the formation of chemical molecules mediating inflammation (pro-inflammatory cytokines), which on the one hand will draw inflammatory cells back into place, exacerbating the inflammation; in addition, persistent inflammatory molecules in the tissue will enter the general bloodstream, causing widespread, generalized inflammatory states throughout the body, thus cellular and tissue damage even in other districts at a distance.
The main consequences of this disorder will, in time, be evident at the cardiovascular level, where an ever-present and ever-active inflammatory state (known as chronic silent inflammation) will predispose and consolidate the formation of atherosclerosis from which cardiovascular accidents such as heart attacks and strokes will originate even years later. This pathological degeneration, will also be aggravated by the presence of other risk factors that, as we shall see, will often if not always be concomitant in a subject with certain decompensations.
Insulin resistance, in a more or less pronounced, more or less symptomatic form, is a condition also associated with increased volume of visceral fat, it follows that in order to achieve a physiological effect on the control of blood glucose concentration (blood glucose), insulin secretions by the pancreas will be required to an increased extent compared with normal, from which we will have hyperinsulinemia and an increasingly pronounced tendency to hyperglycemia, eventually leading to an overt alteration of the glycemic picture that degenerates toward disease Of type 2 diabetes.
Other conditions that very often occur concomitantly with visceral fat accumulation are hypertension and altered lipid patterns (cholesterol and triglycerides), which also contribute to the atherosclerotic damage and cardiovascular accidents we have previously mentioned.
The condition described is a subclinical manifestation, almost always asymptomatic, so it often goes unnoticed, which is called Metabolic Syndrome (MS). This syndrome is very frequently found in the overweight/obese individual with abdominal adiposity of the visceral type (typical abdomen referred to in the jargon as “android” or more vulgarly referred to as “apple-shaped” since it is characterized by a very pronounced round shape and hard to the touch, only in moderate presence of subcutaneous fat that would instead be softer to the touch and also measurable manually).
MS can be diagnosed by examining certain criteria and finding its actual alteration from baseline values, such as measuring a high waist circumference (over 80 cm in women and over 94 cm in men) associated with the concomitant presence of at least 2 additional risk factors, among them: blood pressure, glycemic, and lipid patterns.
However, metabolic syndrome, which if left untreated evolves inexorably toward type 2 diabetes, is a REVERSIBLE condition that can and should be treated first with dietary therapy. Compatible with any other pathological conditions present in the MS sufferer, the elite therapy is based on a high lipolytic and anti-inflammatory diet such as the ketogenic diet could be. With this therapy, resolution of MS could be easily achieved even in a relatively short time while not resorting to the use of medication. Conversely, if left untreated, evolution will be inevitable.
Font
Dr. Gabriele Bedini
Other articles of interest
Cell regeneration and healing with blood plasma