Smart bandages are part of recent technological advances; they can help accelerate wound healing, monitor wounds, and administer treatments.
Smart bandages are emerging as a momentous milestone within the landscape of recent technological advances applied to medicine. Their potential to revolutionize the way we approach wound healing is undeniable.
Furthermore, they offer a perspective where accelerated healing, comprehensive monitoring, and precise treatment delivery converge in a single device. This development is not limited to a simple covering; it represents a symbiosis between materials science, electronics, and artificial intelligence, opening up a range of possibilities to improve patients’ quality of life and optimize healthcare resources. Imagine a future where your wound tells the doctor how it’s healing — without even needing to be touched. That future is already here. For many patients, the idea that a bandage can “talk” to their doctor, detect infections early, and even release medication sounds like science fiction. But it’s real. We’ve entered a new era where healing isn’t passive — it’s intelligent, adaptive, and deeply personalized. And for anyone who’s ever endured a slow or painful recovery, that’s more than innovation — it’s hope.
In essence, smart bandages transcend the functionality of their conventional predecessors. Traditional bandages serve the primary function of protecting the wound from external agents and providing basic support. Smart bandages incorporate sophisticated technology capable of dynamically interacting with the healing process. In this way, these technological devices are established as active systems that not only cover, but also observe, analyze, and respond to the changing needs of the wound in real time.
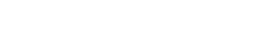
A paradigmatic example of this innovation comes from the work of visionary scientists at the National University of Singapore. Their development has resulted in a smart bandage capable of providing crucial information on the condition of a wound without the need to remove the dressing.
Therefore, this capability represents a significant advance, as constant manipulation of bandages can disrupt the delicate healing process and increase the risk of infection.
Data is collected through a sensor integrated into the bandage, which can measure various physiological parameters relevant to the evolution of the wound.
The significance of this new technology is magnified when considering its potential for the treatment of chronic wounds, a debilitating condition that affects approximately 2% of the world’s population. These wounds, characterized by their persistence and difficulty healing, represent a significant challenge for healthcare systems and a considerable impact on patients’ quality of life.
In this context, smart bandages are presented as a promising tool to address the complexities inherent to these wounds.
Consequently, the benefits offered by smart bandages are multiple and far-reaching:
* Accelerated healing: By optimizing local wound conditions and, in some cases, releasing therapeutic agents, smart bandages can significantly reduce the time required for complete healing.
* Reduced scar formation: By promoting more efficient and organized healing, the formation of prominent scar tissue can be minimized, improving the aesthetic and functional outcome.
* Improved skin recovery: Continuous monitoring and early intervention at any sign of complications contribute to healthier and more complete skin regeneration.
* Infection prevention: The ability to detect early signs of infection and, in some cases, release antimicrobial agents locally significantly reduces the risk of infectious complications.
To fully understand the context in which this innovation emerges, it is pertinent to recall the traditional definition of bandage provided by the World Health Organization (WHO). According to this entity, bandaging consists of wrapping a limb or other body part with bandages or similar materials, with the aim of providing the necessary care and preventing complications.
Smart bandages evolve this definition by actively incorporating technology to optimize this care and prevent complications in an unprecedented way.
The ability of these technological devices to release growth factors directly into the wound bed represents a key mechanism for accelerating tissue regeneration.
Growth factors are proteins that stimulate cell proliferation and differentiation, fundamental processes for tissue repair. By delivering these agents in a controlled and localized manner, smart bandages can positively influence the speed and quality of healing.
Similarly, continuous monitoring of parameters such as temperature, humidity, and pH of the wound microenvironment allows healthcare professionals to obtain valuable information to adjust treatments and prevent potential complications.
The tangible benefits of smart bandages translate into significant advantages for both patients and the healthcare system:
* Faster healing: This reduction in the healing process not only improves the patient’s quality of life by reducing discomfort and immobility, but also leads to a considerable reduction in costs associated with hospitalization and prolonged treatments.
* Designs tailored to patient comfort and characteristics: Research and development in the field of smart bandages also focus on creating devices that are comfortable to wear, flexible, and adaptable to different types and locations of wounds, improving patient adherence to treatment.
* Remote monitoring by treating physicians: Through platforms and mobile applications associated with smart bandages, physicians can remotely monitor the progress of the wound, facilitating early detection of problems, personalizing care, and reducing the need for in-person visits, especially in remote geographic areas or for patients with limited mobility.
* Opportunity for investors, pharmaceutical companies, and hospitals: The acquisition and implementation of this technology represents a strategic opportunity for these healthcare players, allowing them to offer patients an innovative, comfortable, and efficient treatment option. This can translate into improved reputation, greater patient satisfaction, and optimized resources.
The primary function of the smart bandage lies in its ability to dynamically interact with the wound and its environment:
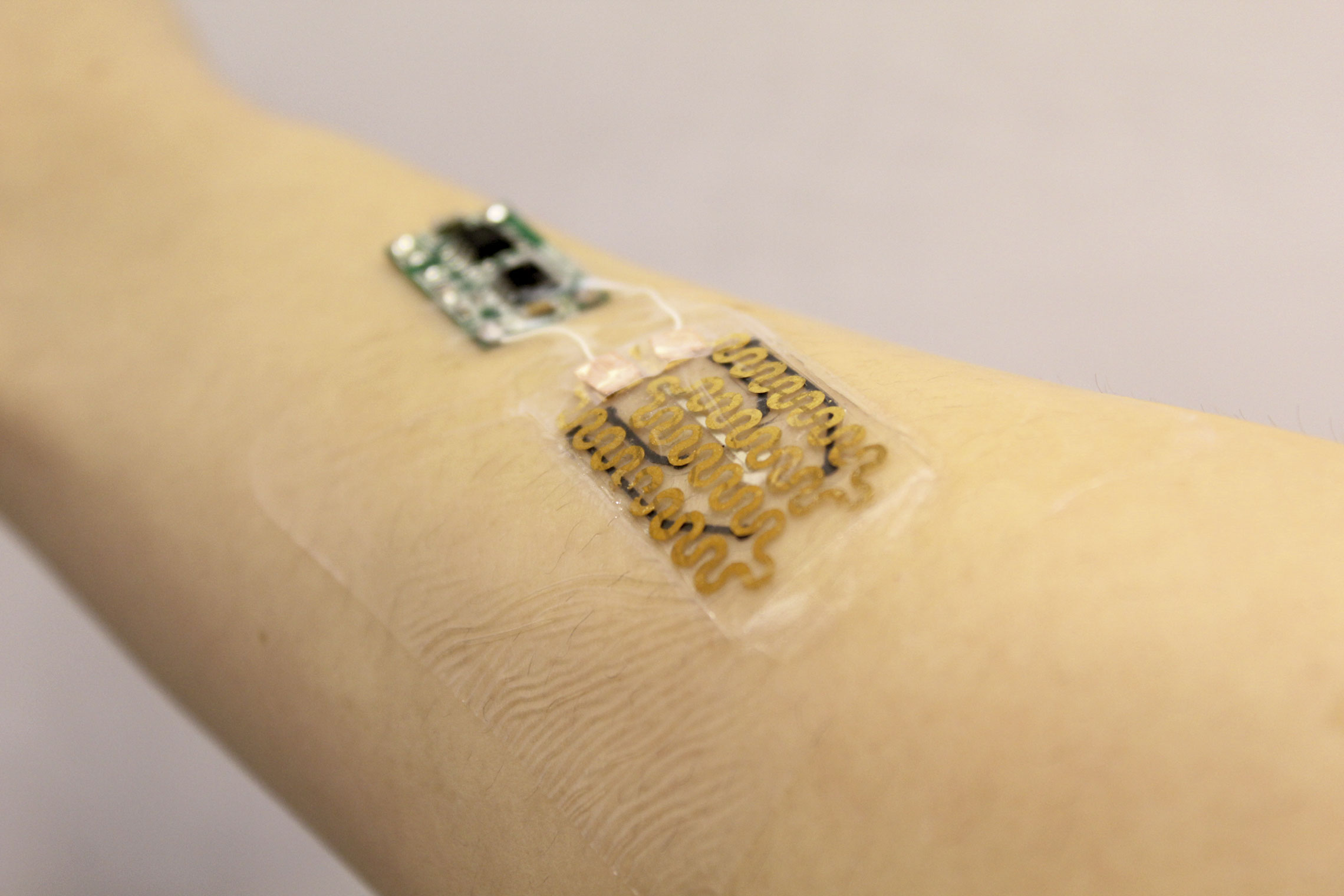
The smart bandage is equipped with sensors capable of detecting subtle changes in electrical conductivity and skin temperature as the wound progresses through its healing process. These variations in biophysical parameters can indicate the presence of inflammation, infection, or poor wound healing, allowing for early and precise intervention.
The smart systems embedded in these dressings have the ability to detect abnormalities, respond to them through controlled drug release or physical stimulation, and inform healthcare professionals about the wound’s condition. This combination of functions is crucial for addressing many of the challenges associated with wound healing, particularly chronic wounds, where the timely detection of complications such as infections is critical to improving clinical outcomes.
To illustrate the diversity and potential of this technology, it is useful to review some specific examples of smart dressings that are under development or already available:
* The smart dressing developed by scientists at the National University of Singapore, mentioned above, stands out for its ability to provide detailed information about the wound without the need to remove the dressing, minimizing interruptions to the healing process and reducing the risk of contamination.
* Another example is a wireless smart bandage that has been shown to accelerate wound healing by approximately 25%. This device uses wireless communication technology to transmit data to an external device, enabling continuous, real-time monitoring.
* A smart bandage that uses tiny LED lights to emit ultraviolet C (UV-C) light represents an innovative strategy for wound sterilization. UV-C light has antimicrobial properties and can help prevent or treat local infections without the need for systemic antibiotics.
Finally, there are smart bandages that employ electrical stimulation and biosensors to increase blood flow to injured tissue. Improving blood circulation is crucial for the delivery of oxygen and nutrients necessary for tissue regeneration, which can significantly accelerate healing, especially in vascularly compromised wounds.
While smart bandages represent an exciting frontier in wound care, it is important to remember the types of conventional bandages that still play a fundamental role in current clinical practice. These traditional bandages are classified according to their primary function and the type of material used.
It is important to understand the types of bandages that currently exist:
The smart bandage itself, although advanced, shares the basic function of protecting or supporting a specific body part, but with the addition of technological capabilities.
There are several types of traditional bandages, each designed for a specific purpose:
* Herringbone: Used to cover large areas of a limb, overlapping the wraps of the bandage obliquely, similar to the scales of a fish.
* Spiral: Used to secure dressings or provide light compression on a limb, with wraps of the bandage partially overlapping upward.
* Recurrent: Ideal for covering distal areas such as the fingers or head, where the bandage is passed from one side to the other, covering the limb and secured with circular wraps.
* Figure-of-eight bandage: Primarily used to immobilize joints such as the ankle or wrist, forming a figure of eight around the joint. * Pretape: A thin, elastic bandage applied directly to the skin before applying a functional or sports bandage, providing a supportive and protective base.
* Functional or sports bandage: Designed to provide support and stability to muscles and joints during physical activity or for injury recovery.
* Compression bandages: Applied to exert controlled pressure on a limb, used in the treatment of edema, venous, or lymphatic insufficiency.
Additionally, bandages can be classified into three main categories based on their presentation:
* Roll bandages: The most common form, available in widths and lengths, and made from a variety of materials such as cotton, gauze, or elastic.
* Triangular bandages: Pieces of fabric shaped like isosceles triangles, versatile for immobilizing limbs, supporting slings, or using as improvised dressings.
* Tubular bandages: Elastic, tube-shaped mesh used to secure dressings on different parts of the body, especially fingers, arms, or legs.
Consequently, the future of smart bandages looks extremely promising and full of transformative potential. Thus, the synergistic convergence of advances in fields as diverse as nanotechnology, miniaturized biosensors, and artificial intelligence applied to medicine.
On the other hand, the development of advanced materials will inevitably drive the creation of even more sophisticated, multifunctional bandages tailored to the individual needs of each patient.
It is highly likely that in the near future we will see a wide range of innovative clinical applications for smart bandages in various fields of medicine.
Furthermore, these applications could range from the advanced treatment of complex wounds and extensive burns to the continuous, noninvasive monitoring of important vital signs and the personalized delivery of medications through the skin, offering an alternative to traditional administration routes.
Finally, continued research and multidisciplinary collaboration between materials scientists, biomedical engineers, and specialized clinicians are absolutely critical to fully realize the potential inherent in this revolutionary technology and significantly transform the way patient care is delivered in the near future.
I invite you to read another interesting article:
Insulin: 1 Century of Changing Lives
Font:
https://medac.es/blogs/sanidad/tipos-de-vendajes
https://www.expomedhub.com/nota/innovacion/los-vendajes-inteligentes-que-aceleran-la-cicatrizacion