Uterine Polyps: A Detailed Examination of Its Nature, Etiology, Clinical Manifestations, and Therapeutic Approach
Uterine polyps are the most common benign pathology in women with abnormal uterine bleeding or infertility.
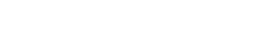
Uterine Polyps: Definition and General Characteristics
A uterine polyps, also known as an endometrial polyp, represents an abnormal proliferation of tissue that projects into the uterine cavity. This growth, which attaches to the uterine wall by a narrow base called a pedicle or a broader stalk, is composed primarily of the inner lining of the uterus, the endometrium.
Histologically, an endometrial polyp is characterized by an epithelial covering surrounding an internal structure made up of varying amounts of stroma (supporting tissue), endometrial glands, and blood vessels.
Although the most common location of these growths is the lumen of the uterine cavity, it is important to note that they can sometimes originate in the cervical canal (the tube that connects the uterus to the vagina) or even extend into the vagina.
The age range in which the presence of uterine polyps has been documented is broad, ranging from early adolescence (12 years) to old age (81 years). However, the prevalence of this condition increases significantly with age, being more common in women between 40 and 65 years of age.
The rarity of uterine polyps in the adolescent population is notable. In the context of polyps that present with symptoms, a tendency toward increasing prevalence with age is observed, and various studies suggest a higher incidence in premenopausal women compared to those who have already gone through menopause.
In fact, uterine polyps are considered the most common benign pathology in women who experience abnormal uterine bleeding or who have difficulty conceiving (infertility), these being the two cardinal symptoms associated with their presence.
The size of uterine polyps can vary considerably, ranging from millimeters in size, which often go unnoticed, to several centimeters in diameter.
It is crucial to note that the impact of polyps on female fertility depends largely on their size and location. While some small polyps may not interfere with reproductive capacity, others, especially those that are larger or located in strategic areas of the uterus, can hinder the transport of sperm to the egg and impair embryo implantation in the endometrium.
Risk Factors Associated with the Development of Uterine Polyps
Several factors have been identified as potential contributors to the development of uterine polyps, although the precise etiology of this condition is not yet fully understood. Among these risk factors, hormone levels play a key role. First, estrogens, female sex hormones produced primarily by the ovaries and, to a lesser extent, by the adrenal glands, have been associated with an increased risk of developing endometrial polyps. During pregnancy, the placenta also contributes to the synthesis of these hormones.
The influence of estrogens on endometrial growth suggests a direct link with the abnormal tissue proliferation that characterizes uterine polyps.
Second, tamoxifen, a widely used and proven effective drug for the treatment of breast cancer, has been implicated in the development of uterine polyps in a significant percentage of postmenopausal women.
Studies indicate that between 2% and 36% of women receiving tamoxifen treatment may develop uterine polyps. It is believed that the antiestrogenic effect of tamoxifen on breast tissue may have a paradoxical estrogenic effect on the endometrium, stimulating its growth and the formation of polyps.
Third, hormonal treatments in postmenopausal women, intended to relieve symptoms associated with estrogen deficiency, have also been considered a potential risk factor for the development of uterine polyps.
The administration of exogenous estrogens can stimulate endometrial growth and, consequently, increase the likelihood of polyp formation.
Fourth, advanced age has been identified as an independent risk factor for the development of uterine polyps. As women age, hormonal changes and other physiological processes may increase susceptibility to the development of these formations.
Fifth, while some early studies suggested a possible association between hypertension and obesity and the development of uterine polyps, more recent research tends to conclude that, on their own, these factors cannot be considered direct causes or significant risk factors for their development.
However, it is important to consider that both hypertension and obesity may be related to hormonal imbalances that could indirectly influence the risk of developing polyps.
Finally, some rare diseases, such as Lynch syndrome, an inherited disorder that increases the risk of several types of cancer, and Cowden syndrome, a genetic condition characterized by the growth of multiple hamartomas, have been associated with an increased risk of developing endometrial polyps.
These associations suggest the existence of underlying genetic and molecular mechanisms that may predispose certain individuals to the formation of uterine polyps.
Clinical Manifestations of Uterine Polyps
When uterine polyps present clinically, their most common and relevant symptoms are alterations in the uterine bleeding pattern.
First, abnormal uterine bleeding, often described by patients as vaginal bleeding outside the regular menstrual cycle, is the most prevalent symptom, affecting a considerable percentage of women with polyps, ranging from 64% to 88%.
This bleeding can present in various forms, sometimes making it difficult for the patient to interpret.
Within the spectrum of abnormal uterine bleeding, menorrhagia, characterized by excessively heavy and prolonged menstrual periods, is one of the possible manifestations. This heavy menstrual bleeding can significantly interfere with a woman’s quality of life, causing fatigue, anemia, and emotional distress.
Another presentation is metrorrhagia, defined as vaginal bleeding that occurs outside of regular menstrual periods. Generally, this bleeding is not as heavy as menorrhagia, but its unpredictable occurrence can cause concern and require medical evaluation.
Uterrhagia is a particularly common symptom in premenopausal women with endometrial polyps, although it is also a common presentation in postmenopausal women, where any vaginal bleeding is considered abnormal and should be investigated.
Finally, vaginal bleeding after intercourse (coitorrhagia) is another symptom that may be associated with the presence of uterine polyps, especially those located in the cervical canal or near the internal cervical os. Friction during intercourse can irritate the polyp and cause bleeding.
Therapeutic Approach to Uterine Polyps
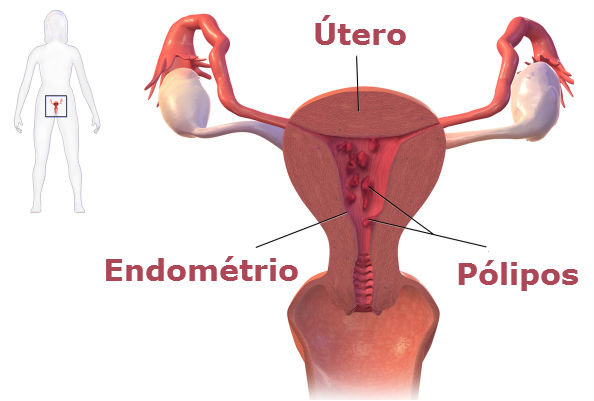
Once a uterine polyp has been diagnosed, the treatment of choice is primarily surgical, with the goal of removing the polyp and, in some cases, obtaining tissue for histopathological analysis.
One of the surgical techniques used is uterine curettage (scraping), a procedure that involves dilating the cervix and inserting an instrument called a curette to scrape the walls of the uterus and remove abnormal tissue, including the polyp.
While curettage can be effective in removing polyps, it has the limitation of being a “blind” procedure, meaning the surgeon does not have direct visualization of the interior of the uterine cavity, and therefore, there is a higher risk of incomplete resection or damage to the uterine walls.
A more precise and recommended surgical technique is hysteroscopic resection. This minimally invasive procedure is performed by introducing a hysteroscope, a thin telescope with a light source and camera, through the cervix into the uterine cavity.
The hysteroscope allows the surgeon to directly visualize the polyp, identify its implantation base, and resect it in a controlled manner using small instruments inserted through the hysteroscope channel. Hysteroscopic resection offers several advantages over curettage, including greater precision in polyp removal, a lower likelihood of recurrence, and the ability to obtain a polyp-specific tissue sample for histopathological analysis.
In specific situations, such as in perimenopausal women with polyps that, upon microscopic analysis, suggest a risk of malignancy (although malignant transformation of uterine polyps is rare), hysterectomy (surgical removal of the entire uterus) may be considered a therapeutic alternative.
Hysterectomy ensures complete removal of endometrial tissue and therefore significantly reduces the risk of recurrence or the development of uterine cancer.
Strategies for Early Detection and Preventive Considerations
Finally, regarding the prevention of uterine polyps, establishing specific preventive measures is difficult due to the uncertainty surrounding their exact causes. Since hormonal factors appear to play an important role, maintaining a healthy hormonal balance could be beneficial, although there are no definitive preventive strategies. Therefore, the main recommendation is to undergo regular gynecological checkups.
These checkups allow for the early detection of any uterine abnormalities, including polyps, through physical examination, transvaginal ultrasound, and, if suspected, diagnostic hysteroscopy.
Early detection of uterine polyps facilitates timely treatment and can prevent the onset of symptoms and associated complications.
It’s important for you to know that although uterine polyps are generally not life-threatening or cancerous, they can make it difficult for couples to conceive.
Some rare diseases, such as Lynch syndrome or Cowden syndrome, are associated with an increased risk of developing endometrial polyps.
Always take care of your health with a unique and efficient service. Visit Pharmamedic.
I invite you to read another interesting article:
Mental Wellness: 1 Real Future with AI
Font:
https://www.mayoclinic.org/es/diseases-conditions/uterine-polyps/diagnosis-treatment/drc-20378713